Have you ever gone to your doctor because you are sick and feel you need antibiotics, only to be told that antibiotics won’t work for your illness? It can be frustrating, especially when you’re already feeling down.
Your frustration is understandable. Patients sometimes expect to be prescribed antibiotics because of past experience. However, antibiotics are only effective for infections caused by bacteria, not against viral infections. Taking unnecessary antibiotics can cause unwanted side effects and can lead to antibiotic resistance.
Understanding the difference between bacteria and viruses, why antibiotics only work for treating bacterial illnesses, and how to manage viral diseases at home can help you make an informed decision about your health. This knowledge may also help ease your frustration.
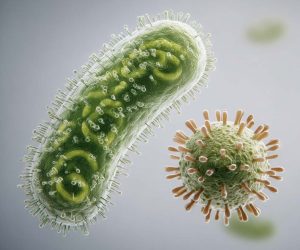
Viruses are tiny, microscopic germs that can make you sick. Viruses consist of an outer coat called a capsid that covers the inner genetic material. Viruses aren’t considered living organisms because they can’t survive without a host. Viruses can’t replicate on their own. Instead, they hijack cells from their host, such as humans, to reproduce. Viruses almost always cause illness.
Most viral infections resolve on their own within a couple of weeks, while other viruses, such as COVID-19, can take several months to subside. Some chronic viruses, like HIV, require long-term treatment with antiviral medications.
Bacteria, on the other hand, are microscopic, single-celled organisms that can survive on their own. They have a cell wall that protects the inner reproductive material, which consists of DNA.
Most bacteria are harmless to humans; in some cases, they can even be helpful. Our gut is full of “good” bacteria that help us digest food.
However, some bacteria can make us sick by producing toxins. Bacteria can cause just a mild illness, or they can land you in the hospital with septicemia, which is a blood infection.
Bacterial infections typically don’t resolve on their own; they require treatment with an antibiotic.
Antibiotics are only effective in treating bacterial infections. Some antibiotics destroy the bacteria’s cell wall or their inner DNA, while others work by interfering with crucial protein production.
Antibiotics aren’t effective in treating viral illnesses since viruses are made of different components. Viruses don’t have cell walls or make proteins on their own.
Using antibiotics to treat viruses can lead to antibiotic resistance, which means the antibiotic loses its effectiveness against bacteria.

Antibiotic resistance is a serious global health crisis, according to the World Health Organization. Millions of people die each year from bacterial infections that don’t respond to antibiotic treatment.
Bacteria can evade the effects of antibiotics through genetic mutation – the bacteria’s genes change in a way that prevents the antibiotic from working. When an antibiotic is given to a person, the susceptible bacteria are killed, but those with genetic mutations survive and reproduce.
The more we use antibiotics, the more resistance occurs. It’s scary to imagine a world without effective antibiotics.
It’s essential to take antibiotics only when they are truly necessary. Taking antibiotics for viral infections is not only ineffective, but it can also cause antibiotics to stop working for bacterial infections.
Bacterial and viral illnesses share many of the same symptoms, including fever, cough, and runny nose. Bacterial infections usually cause more intense symptoms.
Your doctor can determine whether you have a bacterial or viral infection by conducting a thorough history and physical examination, obtaining cultures, and, in some cases, performing additional laboratory tests. If your doctor diagnoses you with a bacterial infection, they will prescribe antibiotics to treat it.
It’s essential to take all of your antibiotics as directed. If you only take your antibiotic until you start to feel better, the infection could return, or antibiotic resistance could develop.
Respiratory viral infections typically begin to improve around the fourth day and are usually much better within a week. It can take a couple of weeks to feel completely back to normal. Most viral symptoms can be effectively treated at home.

If your symptoms worsen over time, if you have a fever for more than 48 hours, or if you don’t feel better after a week, it’s time to see your doctor.
Vaccines are a valuable tool for preventing viral infections or reducing the severity of their symptoms. There are effective vaccines for COVID-19, influenza, measles, chickenpox, as well as many other viruses.
